The incision is shown in blue for a lateral thoracotomy. The patient's arm is over their head, which rotates the scapula. The incision divides the rhomboid major, latissimus dorsi and serratus anterior.
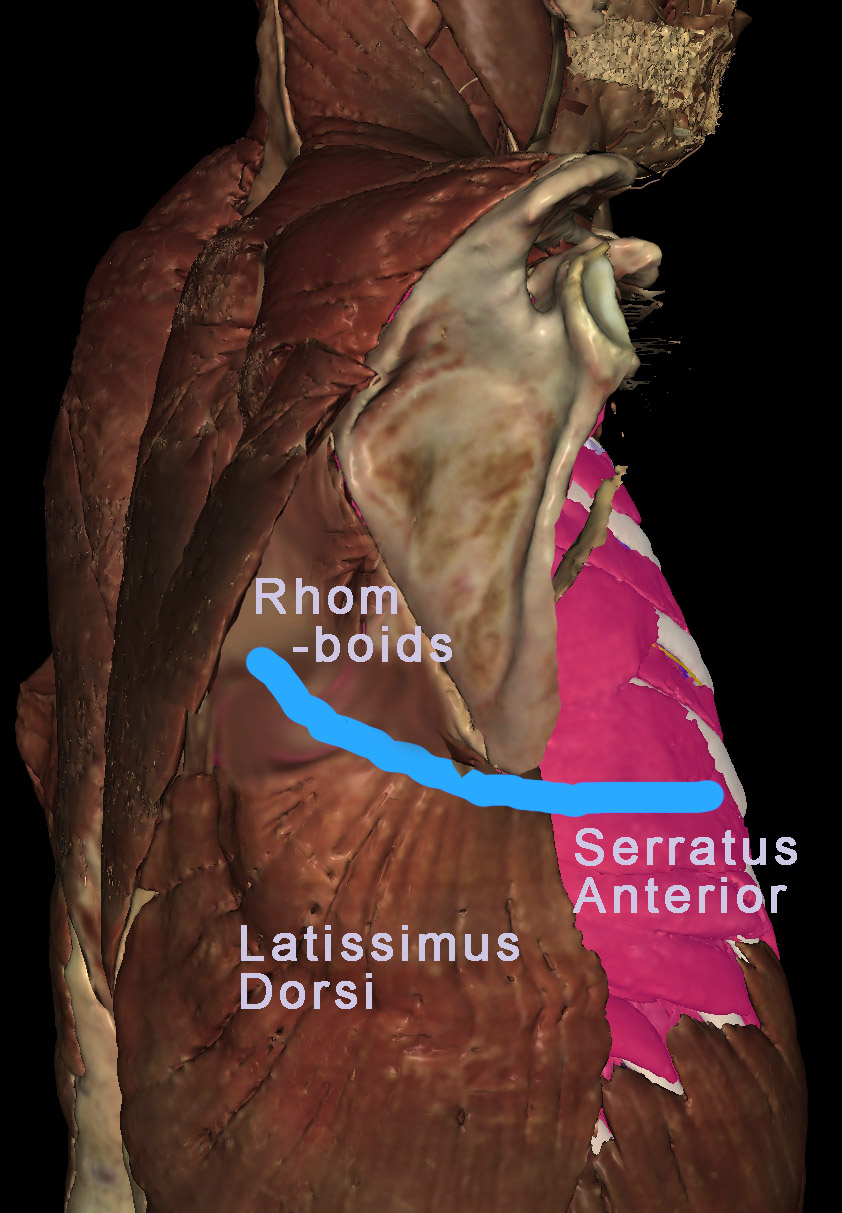
To emulate this incision, dissect the latissimus dorsi and serratus anterior. (Note: the scapula is not rotated in VH Dissector; the above image was Photoshopped).
What do the latissimus dorsi, rhomboids, and serratus anterior do?
Principal functions: latissimus dorsi - adduct and extend the arm; rhomboids - medially rotate and retract the scapula (move it medially); serratus anterior - laterally rotate and protract the scapula (move it laterally).
The rib cage and intercostal muscles are exposed. The external and internal intercostal muscle of the fourth intercostal space need to be divided from the ribs.
Should you make your incision along the superior border of the rib or the inferior border? Why?
An incision along the superior border avoids the neurovascular bundle traveling just inferior to each rib.
Dissect the external oblique and then the internal oblique. Zoom in to see the intercostal nerve (yellow), vein (blue), and artery (red) peaking out below each rib.
Typically, the surgeon would use retractors to spread open the intercostal space. For a better view remove ribs 3, 4, 5, and 6. This will give you a better view of the neurovascular bundle associated with each rib. Dissect the nerves, arteries and veins. The right lung is seen superiorly and the diaphragm inferiorly. Mouse over the lungs to identify the three lobes and find the borders between them. Use the highlight tool to de-highlight the middle lobe.
To view the lungs, the surgeon has to divide the costal pleura creating a pnuemothorax. Why? What will happen to the lung?
The lung will collapse, because 1) air pressure will equalize between the inside and outside of the lung, and 2) elastin fibers in the lung will contract. Think of the pleural membranes as a balloon. Imagine the lung as your fist and punch your fist into the balloon (i.e., inflate the lung) until the membrane covering your fist meets the membrane opposite it. To avoid compressing the air in the "balloon", you would remove air as you expand the lung. Normally, the lumen of the pleural membranes (the balloon) is a vacuum and air in the lungs keeps the visceral pleura of the lung pressed against the parietal pleura that lines the ribs, diaphragm, and mediastinum. When the rib cage expands and the diaphragm moves interiorly, space is created for the lungs to expand, and air is drawn into the lungs. Dividing the pleura allows air to enter and eliminate the vacuum. The lung will collapse to ~ 1/3rd it's normal size. The anesthesiologist can remove more air to make the lung smaller still, affording the surgeon lots of space.
Dissect the middle lobe. Identify the bronchi and arteries of the middle lobe. Notice how arteries and bronchi identified by VHD branch together. If all the bronchi could be colored, each artery would have an accompanying bronchus. Be careful to preserve the lobar artery and bronchus, as you dissect all the branches labeled "segmental".
What is the functional significance of bronchi branching together with arteries?
As the airway and artery branch in parallel, they get narrower and narrower. When the airway is at its thinnest, so is the artery (now a capillary), and gases exchange between the two. The lung is divided into lobes and bronchopulmonary segments. The first branch of the trachea defines left vs. right lung. The second branch defines a lobe. The third branch defines a bronchopulmonary segment.
Dissect the superior lobe. Now you see veins in addition to the arteries. Veins do not branch in parallel with bronchi. Instead, they travel between bronchopulmonary segments. Avoiding tbe veins, preserve branches labeled "lobar" as you dissect arterial and bronchial branches labeled "segmental".
Dissect the lower lobe. Rotate the image to appreciate the distribution of airways, arteries, and veins. Leave the veins and dissect anything labeled "segmental".
Observe the bronchopulmonary lymph nodes, colored green. Note that they are wrapped around the main and lobar bronchi. This region is the hialus of the lung (the region where vessels and airways enter/leave the lung). Dissect the lymph nodes.
Trace the veins to where they enter the left atrium of the heart. The muscle of the left atrium (myocardium) is colored pink and the lumen of the atrium is brown. Dissect each vein. Rotate the image to find two rings of atrial myocardium. This where the veins entered the left atrium. Use the index to look up the right pulmonary veins. Toggle them on and off to confirm they enter the heart at this location. It will help to rotate the image as you do this.
By now, your dissection should look something like this. For clarity, we highlighed the superior vena cava and de-highlighted the superior lobar artery. This view looks head-on at the hilum of the right lung. The hilum is bounded by the superior vena cava, arch of the azygos vein and azygos vein. Mouse around to identify the: pulmonary artery; superior, middle, and inferior lobar arteries; trachea; main (primary) bronchus; superior, middle, and inferior lobar (secondary) bronchi . Determine which primary branch is most anterior. The pulmonary veins have been removed from this view of the hilum. To confirm they lie inferior to the airway and artery, infer their position by re-identifing the left atrium, as viewed through anular rings of myocardium.
Which regions are drained by the arch of the azygos vein?
The posterior walls of the chest and abdomen.
Bonus question: In what order do you imagine a surgeon would divide the structures within the hilum?
Historically, the surgeon divided the artery first, because it is anterior most and exposes the main bronchus. After dividing the bronchus, the pulmonary veins are divided. The logic was that if you divide the veins first, the arterial pressure would increase too much. Although true for removing other organs, pulmonary arterial pressure is low to begin with. Consequently, the increased blood pressure is not a big factor. Current data indicates that cancer is more likely to spread if you divide the artery first. Consequently, surgeons now start with the pulmonary veins and work their way superiorly.
Recall that for artery and bronchi there is one primary branch for each lung and one secondary branch for each lobe of the lung. The next, tertiary branches, define functional subunits of each lobe, known as bronchopulmonary segments.
How would you use this information to perform a partial pneumonectomy?
Instead of dividing the main bronchus and pulmonary artery, you would divide the lobar branches for a lobectomy, or the first segmental (tertiary) branche(s) to remove one (or more) bronchopulmonary segments. By re-inflating a tertiary bronchus, that bronchopulmonary segment is clearly distinguished from the rest of the lobe. This enables removal of the lung without compromising neighboring bronchopulmonary segments
Identify two additional structures near the hilum that might be injured during a surgical procedure to divide the right hilum and its contents: the vagus nerve and the phrenic nerve (the accompanying phrenic artery and vein were not identified by VHD).
What is the consequence of injuring the right vagus nerve?
Parasympathetic innervation would be compromised for the embryonic, right side of the esophagus and abdominal 2/3 of the GI tract.
What is the consequence of injuring the right phrenic nerve?
Paralysis of the right hemi-diaphragm would impair breathing.
Rotate the image to appreciate the three-dimensional relationships. End up with this view to examine the hilum along its edge.