Anatomy Relevant to the Post Operative Craniotomy
by Adam Lawson BA, MSc & Terra Doucette Hiller BA, BSN, RN
Cranial Nerves
There are twelve cranial nerves. The first two arise from the cerebrum; the latter ten arise from the brainstem. Cranial nerves are associated with either sensory or motor nuclei. Sensory nuclei relay information received to other nuclei and to processing centers in the cerebrum or cerebellum. Motor nuclei receive information from higher centers or other nuclei and transmit the information to the appropriate innervation.
-
Cranial Nerve I: Olfactory
- Type: sensory
- Location: Nerve fibers embedded in the mucosa of the nasal cavity travel through a portion of the ethmoid bone called the cribiform plate to meet with the olfactory bulbs. Signals are transmitted to and from the olfactory tracts, which pass through the frontal lobes, to connect with several regions of the temporal lobe.
- Function: The olfactory nerve pathways allow for the sense of smell; signals will ultimately interact with areas of the brain involved in a diverse set of functions (e.g., memory, emotion, taste).
- Dysfunction: Anosmia (loss of smell) or hyposmia (partial loss of smell) can be caused by tumors or growths, which compress the ophthalmic bulb, or by damage to the ethmoid bone that causes shearing of the nerves in the cribriform plate.
-
Cranial Nerve II: Optic
- Type: sensory
- Location: Nerve fibers from the retinae emerge from the posterior eyeballs as the optic nerves and decussate (i.e., "cross") at the optic chiasm becoming the optic tracts. The optic tracts travel through the optic foramina in the sphenoid bone. Signals are conveyed through many tracts before reaching the primary visual cortex in the occipital lobe.
- Function: The optic nerve pathways transmit visual information to the brain; signals from the visual fields of each eyeball are ultimately merged into a single visual field and are, additionally, processed by brain structures involved in a diverse set of functions (e.g., memory, emotion, spatial awareness).
- Dysfunction: Injury or compression of an optic nerve distal to the chiasm will affect the ipsilateral (same sided) visual field transmitted from one eyeball. Damage or compression within the optic chiasm often affects both visual fields either medially (binasal) or laterally (bitemporal). Damage proximal to the chiasm causes loss of vision from one eyeball but affects the entire merged contralateral visual field. Other diseases affecting the optic nerve include: glaucoma, optic neuritis and anterior ischemic optic neuropathy.
-
Cranial Nerves III, IV, VI: Oculomotor, Trochlear, Abducens
- Type: motor
-
Location: They all arise from the midbrain and pons to provide motor control of the six extraocular muscles, the levator palpebrae superioris (controls the eyelid) and the ciliary muscles (controls pupillary constriction and lens accommodation). The trochlear and abducens muscles each control only one extraocular muscle:
- Trochlear (IV) - controls the superior oblique muscle.
- Abducens (VI)- controls the lateral rectus muscle .
-
Function
- Oculomotor (III): Controls of the four of the six eye movement muscles, raises the upper eyelid, controls pupil diameter, and changes lens shape to focus images on the retina.
- Trochlear (IV): Trochlea means "pulley." The nerve is named for the pulley-shaped ligament (the "trochlea") through which the superior oblique muscle passes to allow the eye to look down and outward (intorsion).
- Abducens (VI): Moves the eyeball laterally (i.e., abducts the eye).
-
Dysfunction
- Oculomotor nerve (III) dysfunction prevents almost all the extraocular eye movements excepting eyeball abduction and intorsion. A patient may have an eye that looks inferolaterally ("down and out"), a drooping eyelid (ptosis) and/or pupillary dysfunction.
- Trochlear nerve (IV) dysfunction generally causes the eye to drift upward (due to loss of intorsional and some downward movement) and produces a double-visual field; patients will often move their heads inward (giving a "pathetic" appearance) or far to the side to re-align their visual fields. The trochlear nerve was originally named the "pathetic nerve" for this reason.
- Abducens nerve (VI) dysfunction prevents the eyeball from being able to move laterally (i.e., to abduct). The abducens nerves is often the first cranial nerve to lose function in presence of increased intracranial pressure.
-
Cranial Nerve V: Trigeminal (Latin: "three born at the same birth")
- Type: sensory and motor
-
Location: three large branches, which arise from the lateral pons:
- Ophthalmic branch (V1) - conducts sensory signals from the upper face: cornea, ciliary body, iris, lacrimal glands, conjunctiva, nasal mucosal membranes, eyelids, eyebrows, forehead, and nose bridge.
- Maxillary branch (V2) - conducts sensory signals from the middle face: cheek, lower eyelid, lateral nose, upper jaw, teeth, palate, nasal cavity, and sinuses (e.g., pterygoid region, maxillary sinus).
- Mandibular branch (V3) - conducts sensory signals from the lower and lateral face: lower lip skin, chin, ear, lower jaw teeth and the tongue; conducts motor signals to several swallowing and chewing muscles such as: temporalis, masseter, pterygoids, anterior part of the digastric muscles , tensor tympani, and tensor veli of the palatine muscles.
- Function: Provides tactile information (such as pressure, temperature and pain of the face and mouth) and activates the muscles of mastication.
- Dysfunction: Results in face muscle atrophy and/or a syndrome known as trigeminal neuralgia in which a painful, brief facial spasm or tic travels down the face along the route of the trigeminal nerve.
-
Cranial Nerve VII: Facial
- Type: sensory and motor
-
Location: It arises from the pons as it meets the medulla; branches of the nerve conduct sensory signals from the anterior two thirds of the tongue, upper pharynx, and earlobe. It conducts voluntary motor signals to the face muscles and parasympathetic signals to the salivary and lacrimal glands.
- The facial nerve passes through several canals in the temporal bone; it runs through more distance of bone than any other nerve.
- Function: They permit deep pressure sensation over the face and receive taste information from the receptors along the anterior two-thirds of the tongue. They control the muscles of facial expression in the scalp, face and near the ear. They also stimulate the flow of saliva and tears.
- Dysfunction: Asymmetrical loss of facial expression, taste, crying, and salivation may occur. "Bell's palsy" is a paralysis of facial motor neurons that may be caused by inflammation of this nerve as it runs through bone.
-
Cranial Nerve VIII: Vestibulocochlear (a.k.a, auditory nerve, acoustic nerve)
- Type: sensory
-
Location: has two divisions:
- Cochlear portion - its proximal fibers are known as the spiral ganglion; embedded in the cochlea, they conduct the interpreted signals of sound to regions of the medulla, pons, and temporal lobe.
- Vestibular portion - its proximal fibers are known as vestibular ganglion; embedded in the semicircular canals of the inner ear , they conduct the interpreted signals of canal orientation to the pons, medulla oblongata, medulla spinalis (spinal cord), and vermis of the cerebellum.
-
Function
- The cochlear divisions are likely involved in the ability to determine pitch and the locations of sounds in space. The forebrain structures with which they communicate are likely involved in the interpretation of sounds (e.g., language).
- Vestibular divisions convey information from the inner ear about the orientation and movement of the head to help keep equilibrium (i.e. balance).
-
Dysfunction:
- Cochlear division dysfunction will lead to a loss of hearing and/or tinnitus
- Vestibular dysfunction can lead to a false sensation of motion (vertigo), motion sickness, or an involuntary movement of the eye (nystagmus).
-
Cranial Nerves IX, X: Glossopharyngeal, Vagus
- Type: sensory and motor
-
Location: Fibers from these two nerves (along with fibers from cranial nerve XI) intermingle close to where they emerge from the medulla; these fibers conduct motor signals to the constrictor muscles of the pharynx, the stylopharyngeus, and the larynx.
- Glossopharyngeal (IX) - innervates the parotid salivary glands and thetongue.
- Vagus (X) - descends with the common carotid artery and jugular vein to innervate several muscles and organs. Parasympathetic fibers innervate all thoracic organs (e.g., respiratory, cardiac) and all digestive organs before the transverse colon. A few fibers also conduct sensory signals from the dorsal external ear.
-
Function
- Glossopharyngeal (IX): It is abundant in sensory fibers, but it also contains motor fibers. It relays sensory information from the pharynx and the soft palate, provides taste sensation from the posterior third of the tongue, and contains receptors that monitor blood pressure and gas concentrations within blood vessels.
- Vagus (V): Motor signals are conducted to several skeletal muscles involved in speech (via the recurrent laryngeal nerve branch), swallowing, and peristalsis. The vagus nerve is involved in a diverse set of motor, sensory, and parasympathetic functions including: blood pressure, heart rate, sweating, glandular secretion, aortic chemoreception, and opening of the larynx during breathing.
- Dysfunction: Damage to the vagus and/or glossopharyngeal nerves will often cause asymmetrical (or absent) gag reflex; patients may have difficulty swallowing or phonating.
-
Cranial Nerve XI: Spinal Accessory
- Type: motor
-
Location: consists of two branches
- Medullary branch - fuses with the vagus nerve and innervates voluntary swallowing muscles of the soft palate, pharynx, and vocal cords.
- Spinal branch - fibers originate in the lateral gray horns of C1-C5 to innervate the sternocleidomastoid and trapezius muscle.
- Function: It controls muscles of the neck and upper back and permits voluntary swallowing.
- Dysfunction: Asymmetry, atrophy, or fasciculation of shrugs and head turns may imply damage to this nerve.
-
Cranial Nerve XII: Hypoglossal
- Type: motor
- Location: It arises from the medulla and contributes nerve fibers to the muscles of the tongue.
- Function: movement of the tongue
- Dysfunction: Asymmetry, atrophy, or fasciculation of the protruding tongue may imply damage to this nerve.
Vertebral Column
Vertebrae are connected by a number of tendons and ligaments which run from the base of the skull to the coccyx. Intervertebral discs lie between each vertebra to provide the column with flexibility.
There are five types of vertebra:
- Cervical vertebrae - 7 small and highly flexible vertebrae that permit flexion, extension, lateral flexion, and rotation of the head and neck.
- Thoracic vertebrae - 12 vertebrae which permit rotation of the upper torso. Articulation with ribs prevents most lateral flexion and some of the flexion and extension in the sagittal plane.
- Lumbar Vertebrae 5 large, wide, and thick vertebrae which bear the load of the upper body; they permit flexion, extension, some lateral flexion, and some rotation.
- Sacral Vertebrae (a.k.a., Sacrum) - 5 fused and curving vertebrae which lack intervertebral discs; they bear and distribute the weight of the upper torso as they articulate with the pelvic bones.
- Coccygeal Vertebrae (a.k.a., coccyx, tailbone) - 3-5 separate or fused vertebrae which lack intervertebral discs; they act as a site of attachment for several muscles.
Spinal Cord and Spinal Nerves
The spinal cord (a.k.a., medulla spinalis) is the continuation of the brainstem from the medulla oblongata as it exits the skull at the foramen magnum.
The end of spinal cord, called the conus medullaris, terminates at around the level of the first or second lumbar vertebra; long nerve roots branching from it, collectively called the cauda equina (Latin, "horse's tail"), continue through the coccyx.
There are 31 spinal cord nerve segments that innervate the body with both sensory and motor neurons.
-
Cervical segments (C1-C8)
-
Innervation: upper extremities, posterior neck, and posterior head
- C1-C3: neck muscles; posterior scalp
- C3-C5: diaphragm via the phrenic nerve
- C5: deltoid; bicep
- C5-C6 - contribute to the superior trunk of the brachial plexus.
- C6 - wrist extenders
- C7: triceps; contributes to the middle trunk of the brachial plexus.
-
Innervation: upper extremities, posterior neck, and posterior head
-
Thoracic nerves
- Innervation: thoracic cage, lateral portions of proximal lower extremities, and abdomen
-
Lumbar nerves
-
Innervation: deep abdominal muscles; much of the proximal lower extremity
- L1-L5: all leg muscles
-
Innervation: deep abdominal muscles; much of the proximal lower extremity
-
Sacral nerves
- Innervation: pelvic floor, including: bladder, bowels, and sexual organs.
(Click to view animation)
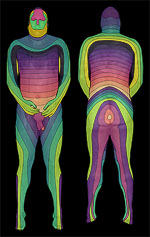
Dermatomes
Dermatomes are the regions of skin surface associated with a particular dorsal root from the spine. Dermatomes facilitate the locating of spinal cord injury during diagnosis; the presence or absence of patient response to touch or pain stimuli at various locations may be referred to specific dermatome stems. Click here for a dermatome chart.