
Weighing in at 250-350 grams (less than a pound), the heart is one of our strongest and most enduring organs.
The heart is enclosed within the mediastinum, the medial cavity of the thorax. About two-thirds of the heart lies to the left of the midsternal line and the balance projects to the right. The broad, flat base, or posterior surface, is about 9 cm wide and is directed toward the right shoulder. The apex points inferiorly toward the left hip.
If you press your fingers between the fifth and sixth ribs just below the left nipple, you can easily feel the beating of your heart where the apex contacts the chest wall. This site is referred to as the point of maximal intensity (PMI).

The pericardium is the membrane that surrounds and protects the heart. This is a double layer membrane. The outer layer is a tough fibrous dense irregular connective tissue. The deeper layer is thinner and more delicate. Its inner structure is the epicardium which is part of the heart wall, too. The pericardium cannot be discerned within your dissection.
Pericardial inflammation is called pericarditis which hinders production of serous fluid and roughens the serous membrane surfaces. Friction with the roughened surface can be heard with a stethoscope.
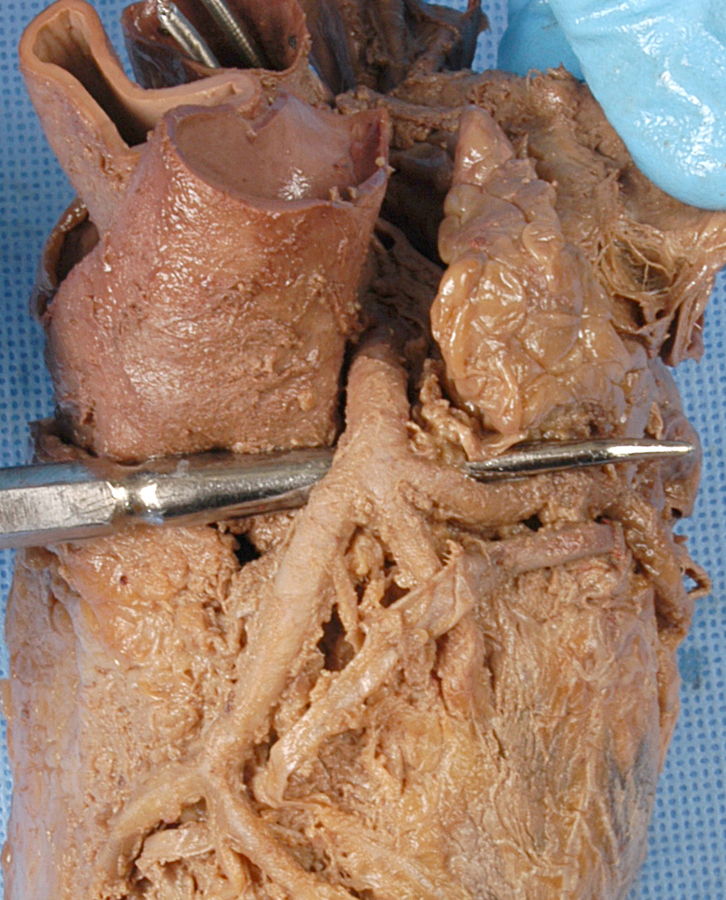
The heart wall has three layers, the superficial epicardium, the medial myocardium, and the deep endocardium. Locate available remnants of the epicardium and the myocardium. The endocardium lines the internal chambers of the heart and is too thin to discern in your dissection. Try to locate the thin epicardium in the cross sectional view. An excellent technique is to highlight the epicardium in the dissection area and look for the highlighted layer to pop up in the cross section. Contrast epicardial thickness with that of the myocardium which is the cardiac muscle tissue that makes up the bulk of the heart and is responsible for its pumping action.
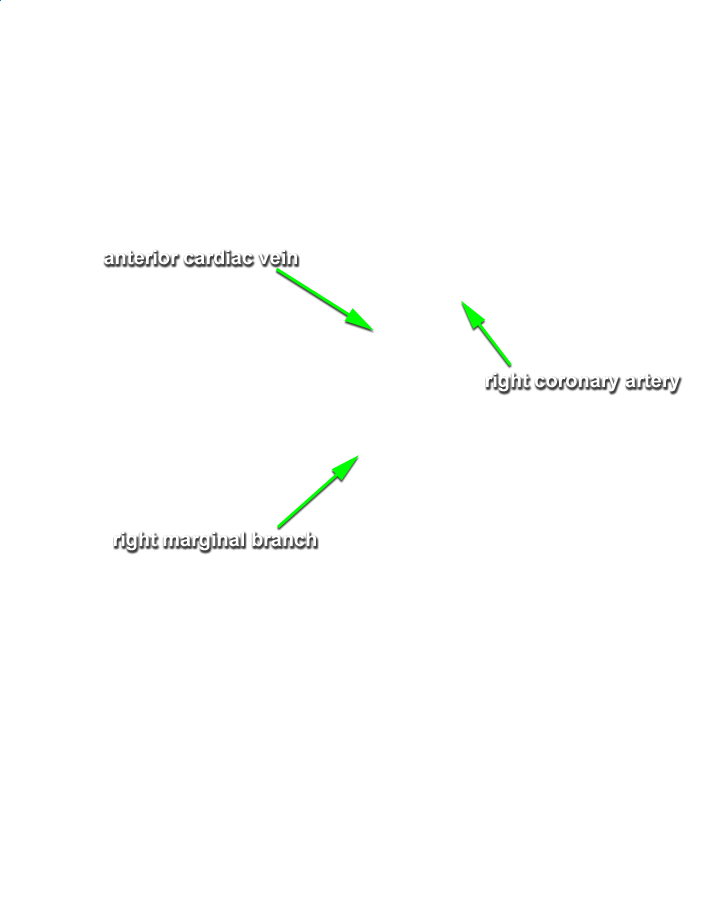
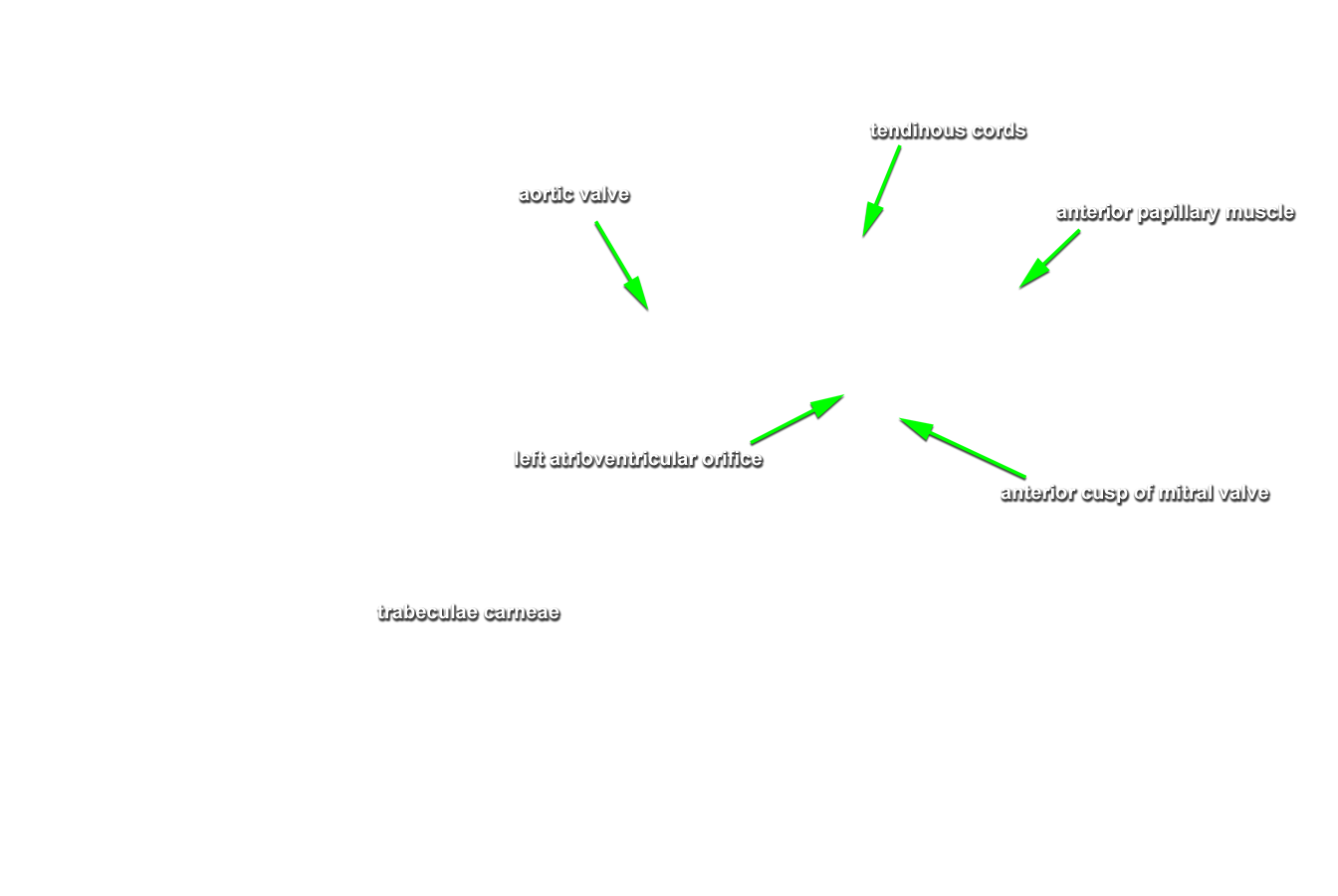
Coronary circulation is the blood supply of the living heart tissue. It is the shortest circulatory route in the body. Locating these vessels in your specimen is difficult so they have been highlighted for you. Identify the following by "mousing over" the highlighted anatomy. If you accidentally click anywhere in the dissection area, you might lose the pre-highlighted coronary vessels. No worries! Just click the "Coronary Circulation" link above and you'll come right back to the same highlighted view of the vessels. Keep track of this critical anatomy on your worksheet images.
Rotate your specimen to examine posterior coronary circulation.
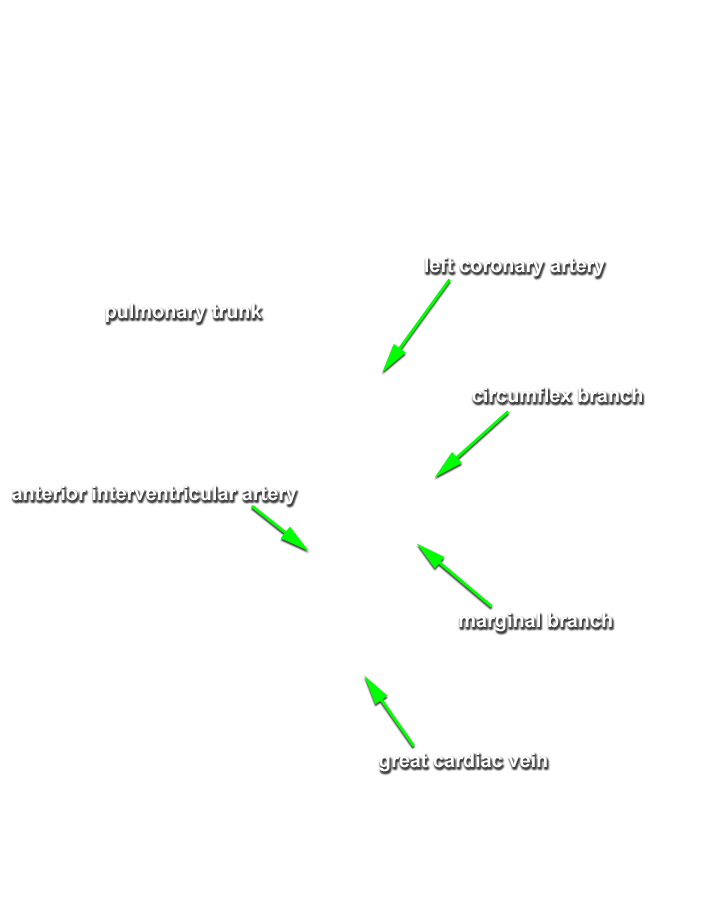
Any coronary arterial blockage can be serious, even fatal. Angina pectoris (literally "choked chest") is thoracic pain caused by a fleeting blood delivery deficiency to the myocardium. It may result from stress induced spasms of the coronary arteries or increased physical demands on the heart. The myocardial cells are weakened by the temporary lack of oxygen but they do not die.
Prolonged coronary blockage is far more serious and can lead to a myocardial infarction (MI), commonly called a "heart attack", or "coronary". Because adult cardiac muscle is amitotic (cells do not divide), any areas of cell death are repaired with non-contractile scar tissue. Whether a person can survive a myocardial infarction depends on the extent and location of the damage. Damage to the left ventricle is the most serious.
Locate the myocardium for each of the following:
As you can see, the cross-sectional plane cuts right through the heart. Locate the following cardiac chambers:

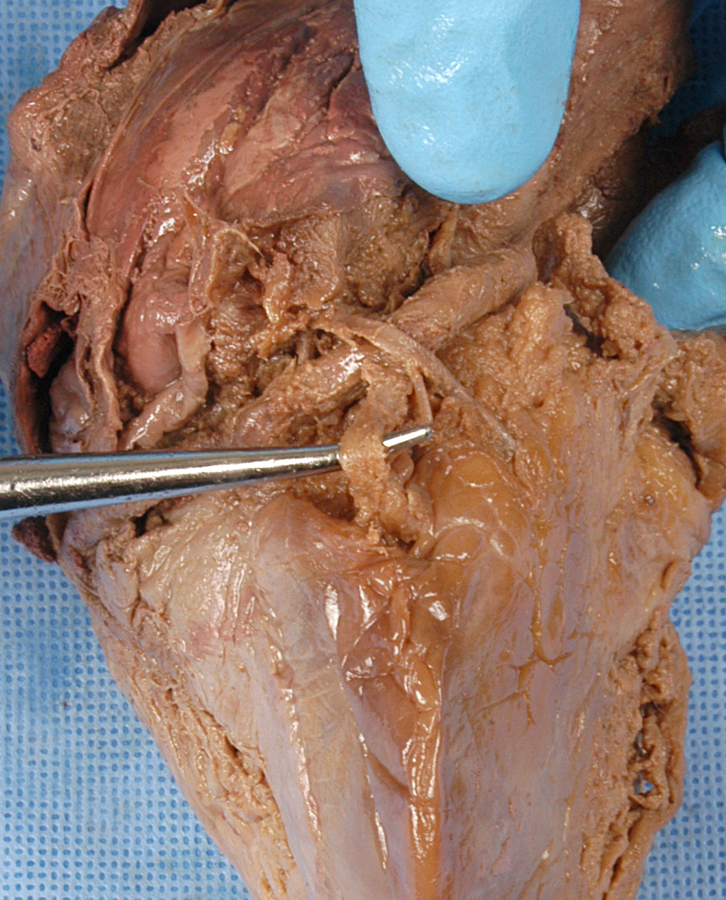
Reveal the heart's internal anatomy by dissecting away the right ventricle myocardium. Identify the trabeculae carneae. These are ridges created by raised bundles of cardiac muscle fibers. Some trabeculae carneae are involved in the cardiac conduction system that cause its rhythmic contraction.
Also present in the right ventricle are the chordae tendineae although they are too detailed to be found within our specimen. The chordae tendineae are tendon-like cords connected to the cusps of the tricuspid valve and to cone shaped extensions of the trabeculae carneae called papillary muscles. The chordae tendineae (tendinous cords) prevent eversion of the atrioventricular valves during ventricular systole. Deoxygenated blood is pumped from the right atrium through the tricuspid valve into the right ventricle. Right ventricular contraction pumps this blood out through the pulmonary valve into the pulmonary trunk on its way to the lungs where gas exchange occurs.
In the cross section, locate the interventricular septum that separates the two ventricles.
Rotate the specimen to the left lateral perspective. This is better for examining the left ventricle. Remember, the VH Dissector has this simply labeled "myocardium" even though it is the left ventricular myocardium. This has already been identified for you but you will need to identify the left atrium.
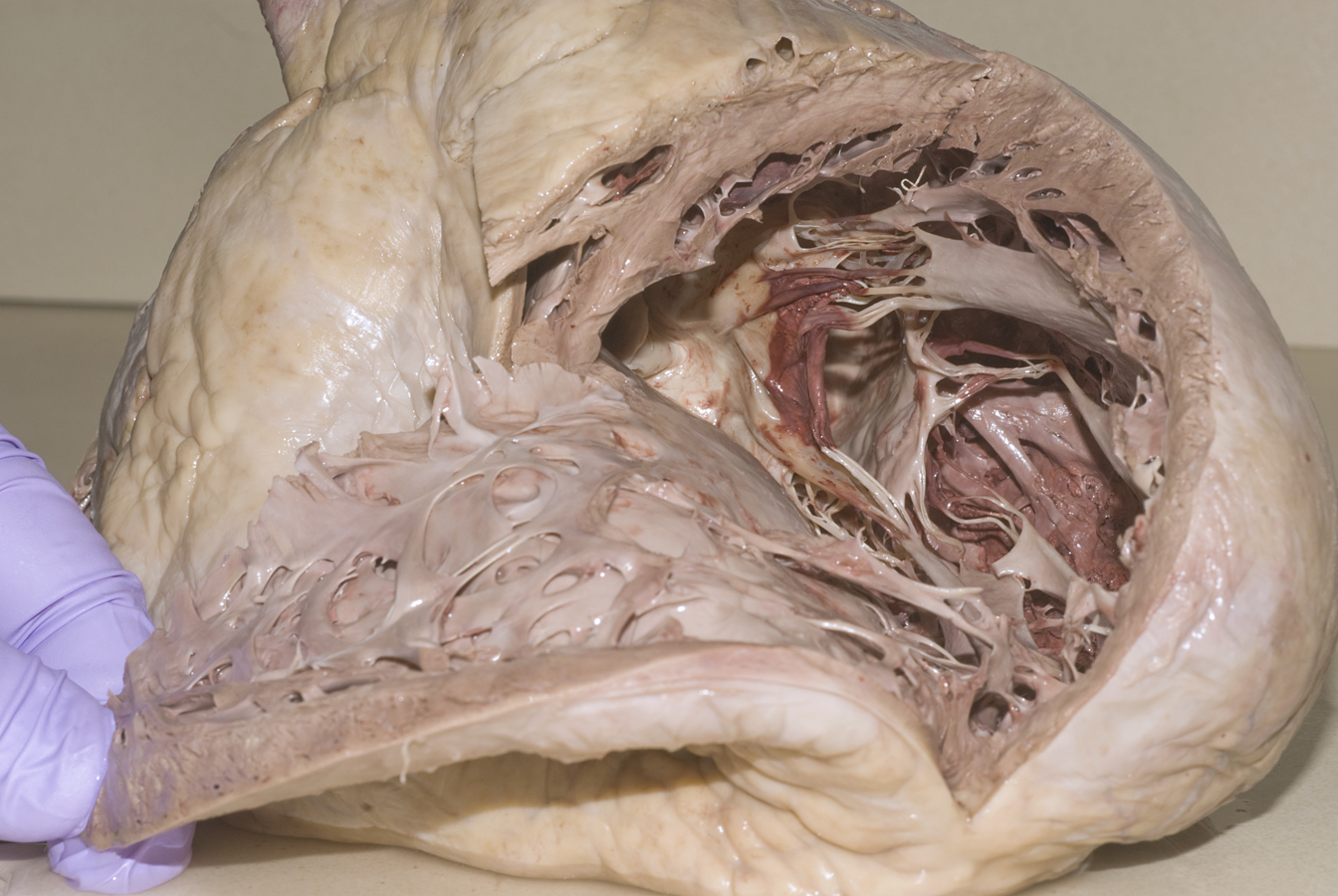
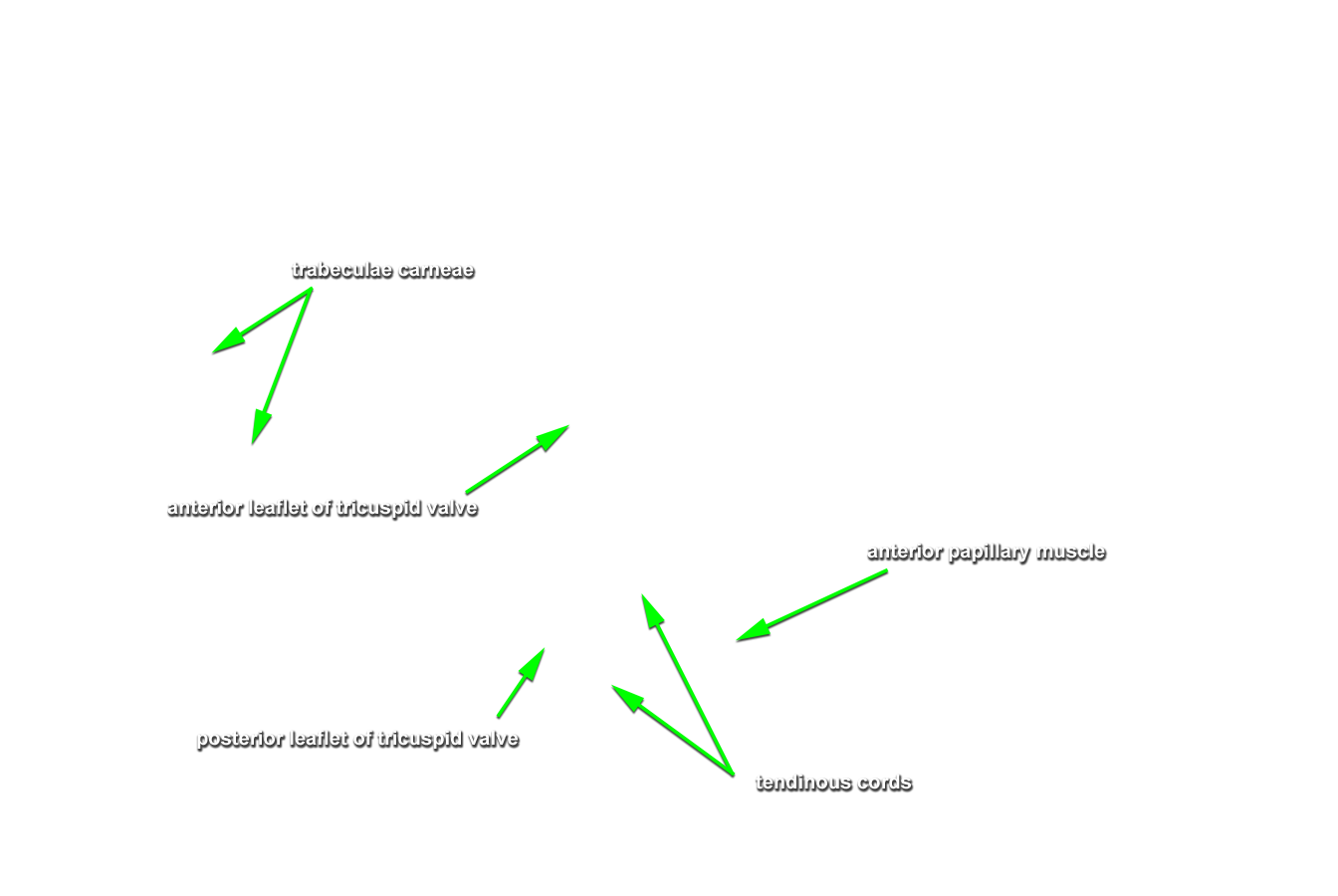
Dissect away this myocardium and examine the interior of the chamber. You will discover papillary muscles and trabeculae carneae here, too.
Blood returns from the lungs into the left atrium which pumps it into the left ventricle through the bicuspid (mitral) valve. The left ventricle then pumps blood out into general systemic circulation through the aortic valve into the ascending aorta. Compared to the right, the myocardium of the left ventricle is thicker, stronger, and requires a constant supply of nutrient rich oxygenated blood due to the magnitude of its task. Some blood is diverted immediately from the aortic arch into the coronary circulation examined earlier. Defects in the chordae tendineae of the mitral valve allow the valve to be everted during ventricular systole thereby "backwashing" blood into the left atrium which significantly reduces cardiac efficiency. Surgically, this can be repaired with an artificial or tissue valve replacement or by "tightening" the cords if the damage is not too extreme.
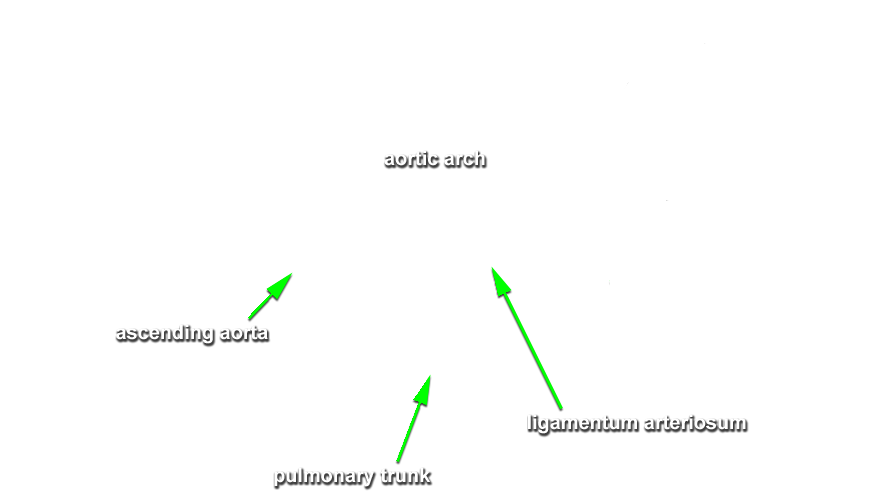
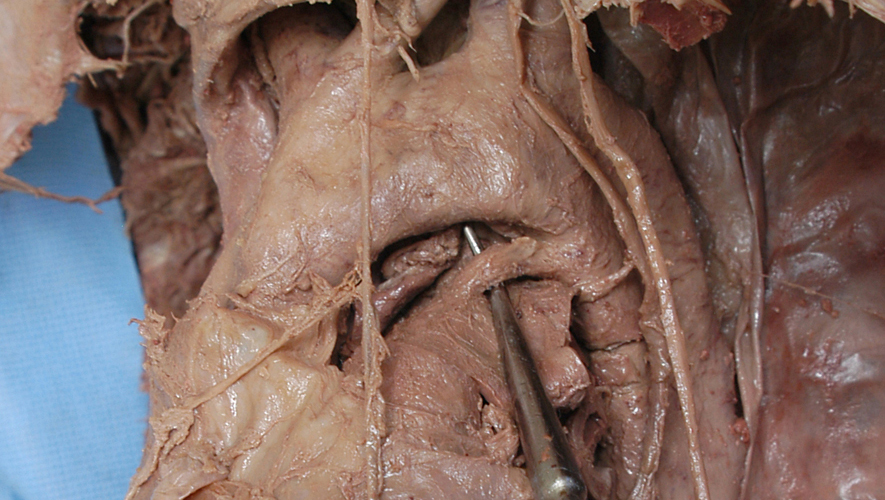
As a fetus blood is shunted from the pulmonary trunk, which conducts blood to our lungs for the rest of our life, directly into the aorta for systemic circulation. Fetal lungs are just developing and not functional till birth. This temporary shunt, or pathway, normally closes shortly after birth leaving behind the ligamentum arteriosum which connects the arch of the aorta and the pulmonary trunk.
You'll find the ligamentum arteriosum along the superior edge of the pulmonary trunk as seen in this lateral perspective.